Serving in the U.S. military is an experience that only the few and the proud can understand. In fact, it’s fewer than ever these days: While nearly 20% of the US population was a veteran in 1980, that number had declined to just 7% by 2017, according to the US Census Bureau. If you are a veteran, you may feel like not many people can understand what you’ve gone through — or what you’re still going through. Indeed, if you’re a veteran struggling with substance abuse, you might feel even more alone. However, substance abuse among veterans is more common than you might think. Even more importantly, there are addiction treatment programs and professionals dedicated to helping veterans find understanding, healing, and a renewed sense of hope and belonging.
What is Substance Abuse?
Put simply, addiction is the compulsion to keep using drugs and alcohol even when your consumption is having a negative effect on your life. The actual amount of drugs or alcohol that is problematic can vary from person to person. Although “binge drinking” is defined as five drinks within two hours for men (and four, for women), some people may find that even one drink turns them into a person they don’t recognize.
Why can some people have a few drinks at the BBQ and continue on with their evening while for others, one beer can turn into an entire lost weekend? It comes down to many factors — and willpower isn’t really one of them.
Substance abuse is no more “your fault” than any other chronic disease like cancer, diabetes, or high blood pressure. While lifestyle choices do play a part, other factors outside of your control — such as genetics and trauma — have a bigger impact on whether you fall victim to addiction.
Veterans & Substance Abuse
Veterans experience substance abuse at rates higher than the general public, according to government studies. For some, this can begin during deployment, where a culture of drinking and drug use pervades daily life. What’s more, one government study found that veterans may put off getting help for substance abuse because of the ongoing stigma in the military and the belief that it may hurt their career. This allows a substance abuse problem to grow and perpetuate, unchecked. Overall, though, many veterans develop substance abuse problems through an attempt to self-medicate trauma or other mental and behavioral health disorders.
Veterans, Trauma, & Mental Health Disorders
Throughout the many branches of the military, the rate of PTSD among veterans has been recorded to be as high as 38%. (According to the National Center for PTSD, that number is only 8% among civilian women and 4% among civilian men.) More than 20% of those veterans struggling with PTSD also struggle with addiction.
Although we are increasingly aware of how PTSD affects our vets, they are susceptible to other mental health disorders as well. One study by the US government found that 31% of returning veterans between 2001 and 2005 had at least one mental health disorder, including depression, anxiety, and more.
Treating Substance Abuse & PTSD
Modern substance abuse treatment is focused on healing the underlying causes of addiction: trauma, and co-occurring mental health disorders. Upon entering residential addiction treatment, clients develop a deep relationship with their treatment team, who work in concert to develop a customized addiction treatment plan that will heal the individual from the inside out. Each individual experiences different addiction treatment modalities depending on their unique emotional wounds. For some, that might include group therapy or CBT (cognitive behavioral therapy) to learn new coping skills. Others may benefit from EMDR (eye movement densensitization reprogramming) for PTSD or even medication for mental health issues.
In residential treatment, clients are supported 24/7 by a team helping them to heal and to build new skills and strategies for life beyond treatment. They also benefit from living alongside others who are experiencing the same process of renewal and transformation.
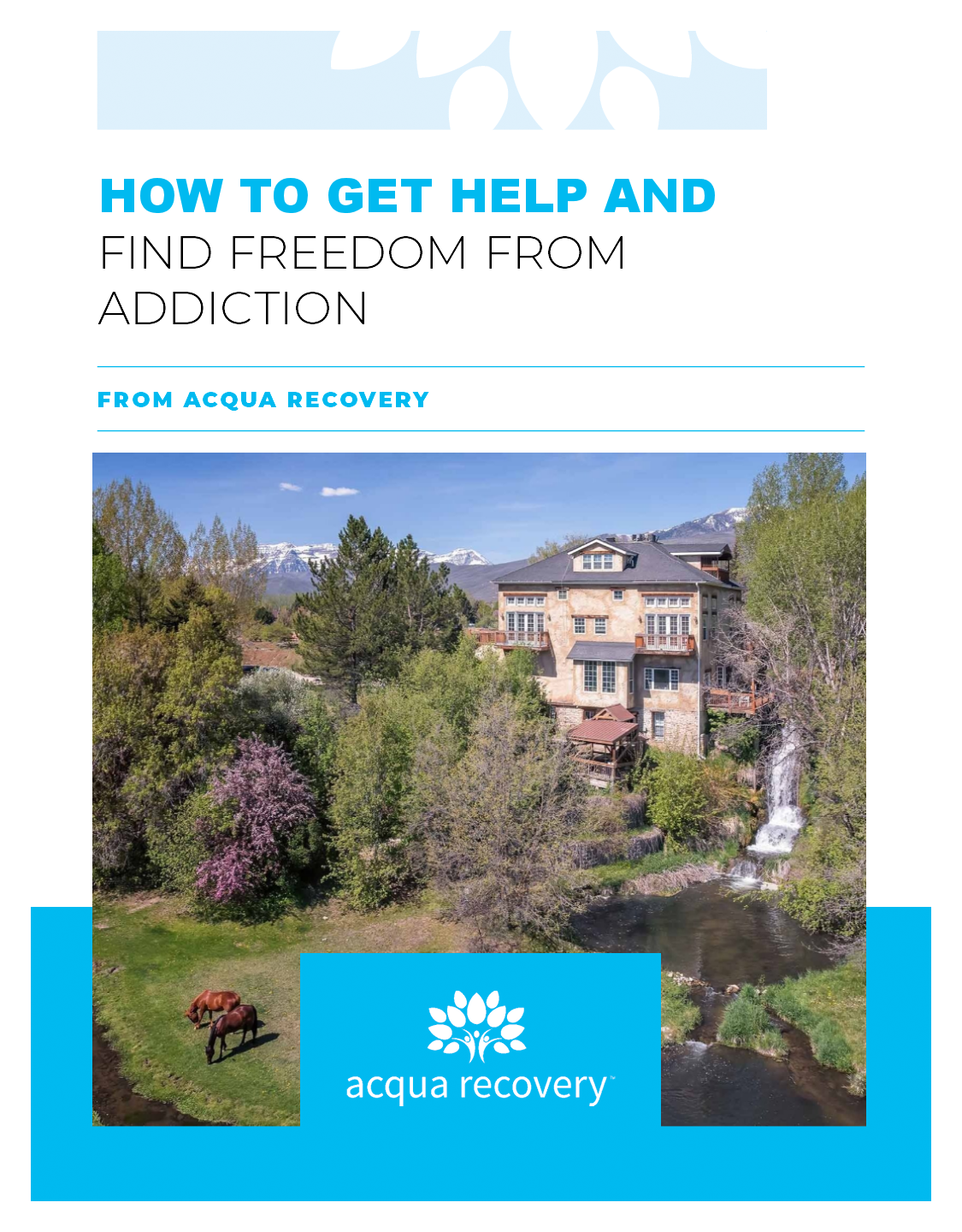
Substance Abuse Treatment for Veterans
At Acqua Recovery, we are in-network with TRICARE, TriWest, and TRICARE EAST — a statement of our commitment to helping veterans find recovery from addiction. If you think that you or a loved one could benefit from caring, expert professional help, give us a call. Members of our admissions team have gone through treatment at Acqua themselves, and they can share their own insight on our addiction treatment programming while listening to your story and helping you figure out the next steps towards true freedom.