BPD and Bipolar Disorder are two different mental health disorders that are oftentimes grouped together. This is due in large part to a lack of understanding surrounding both mental health conditions. It is imperative that those who don’t understand the differences between the two start at a place of understanding them individually. There are a wide variety of differences in BPD and bipolar disorder; these include symptoms, causes, triggers, and even treatment.
What Is BPD?
 Borderline Personality Disorder (BPD) is a serious mental health disorder characterized by pervasive instability in moods, self-image, behavior, and interpersonal relationships. This instability often disrupts family and work life, long-term planning, and the individual’s sense of self-identity. BPD significantly disrupts a person’s quality of life due to its inherent instability.
Borderline Personality Disorder (BPD) is a serious mental health disorder characterized by pervasive instability in moods, self-image, behavior, and interpersonal relationships. This instability often disrupts family and work life, long-term planning, and the individual’s sense of self-identity. BPD significantly disrupts a person’s quality of life due to its inherent instability.
The constant fluctuations in mood, self-image, and behavior make it difficult for individuals with BPD to maintain steady relationships and employment. The unpredictable and often extreme emotional responses can lead to conflicts and misunderstandings with others. Moreover, the lack of a consistent sense of identity often results in feelings of emptiness and confusion, making it hard for these individuals to make long-term plans or decisions. The cumulative effect of these factors often leads to a diminished quality of life, characterized by personal and professional difficulties, isolation, and psychological distress.
BPD is typically characterized by a range of symptoms that cause significant impairment in daily functioning. Key symptoms include:
- Intense mood swings
- Difficulty managing emotions
- Constant fear of abandonment
- Difficulty maintaining stable relationships
- Self-damaging behaviors
- Chronic feelings of emptiness
Additionally, individuals with BPD may exhibit unstable self-image, impulsivity, and may have recurring suicidal thoughts or behaviors. It’s crucial to note that the presence of these symptoms should warrant consultation with a professional for diagnosis and treatment.
BPD is a mental health disorder characterized by unstable moods, behaviors, and relationships. The cause of BPD is generally believed to be a combination of genetic factors, brain structure and function, and environmental influences. Some individuals may have a genetic predisposition to developing BPD, which can then be triggered by stress or traumatic events, including those that might require PTSD treatment in Utah. Certain abnormalities in the brain, such as in the areas that control impulsivity and emotional regulation, may be associated with the disorder. Lastly, adverse childhood experiences such as abuse, neglect, or the loss of a caregiver are frequently reported in individuals with BPD, suggesting a significant environmental component.
BPD is a complex mental health condition and its triggers can be equally multifaceted. Genetic predisposition, brain abnormalities, and environmental factors can all contribute to the onset of BPD. Early traumatic life events such as abuse, neglect, or loss of a loved one can also be significant triggers. Additionally, individuals with BPD may experience heightened sensitivity to emotional stimuli, causing seemingly minor events to trigger intense BPD symptoms. Some of these individuals may also struggle with anxiety, necessitating anxiety treatment alongside BPD interventions. It’s important to note that these triggers can vary widely between individuals, underscoring the complexity of this condition.
BPD is diagnosed based on specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The criteria include the presence of at least five of the following symptoms:
- Intense fear of abandonment (real or perceived)
- A pattern of unstable relationships characterized by alternating between extremes of idealization and devaluation
- Unstable self-image or sense of self
- Impulsive behaviors in at least two areas that are potentially self-damaging
- Recurrent suicidal behavior or threats or self-mutilating behavior
- Affective instability due to a marked reactivity of mood
- Chronic feelings of emptiness
- Inappropriate intense anger or difficulty controlling anger
- Transient, stress-related paranoid ideation or severe dissociative symptoms
What Is Bipolar Disorder?
Bipolar disorder, also known as manic-depressive illness, is a brain disorder; it causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks. It is characterized by episodes of mood swings ranging from depressive lows to manic highs.
The recognition of bipolar disorder dates back to the second century AD, with its detailed clinical features documented by the ancient Greek physician, Aretaeus of Cappadocia. However, the modern understanding of bipolar disorder as a distinct mental illness was not established until the mid-19th century. French psychiatrist Jean-Pierre Falret published an article in 1851 describing what he called “la folie circulaire,” which translates to “circular insanity”—now known today as bipolar disorder. Throughout history, as our understanding of the disorder has evolved, so too has bipolar disorder treatment in Utah, which now includes a combination of medication and therapy to help manage symptoms.
Bipolar disorder is a complicated condition with multiple contributing factors. It is believed that a combination of genetics, the environment, and altered brain structure and chemistry may play a role. People with a family history of bipolar disorder are at a higher risk, suggesting a possible genetic predisposition. Stressful life events or traumatic experiences can trigger bipolar disorder in people with this genetic predisposition. Additionally, imbalances in certain brain chemicals are linked with the disorder. However, it’s important to note that no single cause has been definitively identified, and understanding of this condition continues to evolve.
The exact cause of bipolar disorder remains unknown because of the intricate interplay of multiple factors involved in its onset. Unlike many physical ailments which can be traced to a specific cause, psychiatric conditions such as bipolar disorder are more complicated; they involve complex interactions between genetic factors, brain chemistry, environmental influences, and life experiences. The nature and impact of these factors can vary significantly from person to person, adding another layer of complexity.
Limited understanding about the functioning and interaction of these elements makes it challenging to pinpoint a definitive cause. Additionally, the scientific methods available for such research have significant limitations, preventing us from examining the living human brain in detail. As a result, while we have identified several factors that contribute to the risk of developing bipolar disorder, the exact cause remains elusive.
Bipolar disorder, characterized by extreme mood swings from manic highs to depressive lows, can be triggered by several factors. These include stress, significant life changes, or traumatic events that can precipitate a manic or depressive episode. Furthermore, sleep disruption or irregular sleep patterns can also trigger episodes, making healthy sleep hygiene crucial for those with this disorder. It’s noteworthy that the consumption of alcohol or recreational drugs can exacerbate the condition, often leading to more frequent or severe episodes. Additionally, certain medications, predominantly antidepressants, can trigger mania in individuals with bipolar disorder.
Medications triggering bipolar disorder is a phenomenon known as “antidepressant-induced mania.” The exact mechanism remains uncertain, but it’s believed that these drugs may affect neurotransmitters in the brain such as serotonin and norepinephrine, altering mood regulation and potentially prompting a manic episode. This does not occur in all individuals taking antidepressants and factors such as genetic predisposition may play a role. Consequently, this highlights the importance of careful monitoring when initiating or adjusting antidepressant therapy in individuals with known or suspected bipolar disorder.
The diagnostic criteria for bipolar disorder, as defined by the DSM-5, include experiencing at least one episode of mania or hypomania. Mania is characterized by a period of abnormally and persistently elevated, expansive, or irritable mood; it also includes increased activity or energy, lasting at least one week.
Hypomania shares the same symptoms as mania, but is less severe and lasts for at least four consecutive days. These episodes are often accompanied by depressive episodes, which are marked by feelings of intense sadness, loss of energy, and difficulty enjoying activities, lasting at least two weeks. It’s important to note that these symptoms must cause significant distress or impairment in social, occupational, or other important areas of functioning.
Why Do People Confuse BPD with Bipolar Disorder?
Many people often confuse BPD with Bipolar Disorder due to the overlapping symptoms they share; these include mood swings, impulsiveness, and periods of intense depression or mania. These shared characteristics can make it quite challenging for even experienced clinicians to differentiate between the two without comprehensive evaluation. It’s also relevant to note that both disorders can co-occur, adding another layer of complexity.
Treatment for BPD and Bipolar Disorder
 Treatment for BPD and Bipolar Disorder involves a combination of psychotherapy and medication. Psychotherapy, often referred to as talk therapy, includes Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT). These methods of care are beneficial for managing symptoms of BPD and Bipolar Disorder. Medication, such as mood stabilizers, antipsychotics, or antidepressants, may be prescribed based on individual symptoms. Treatment plans should be personalized under the guidance of a mental health professional, and may require adjustments over time.
Treatment for BPD and Bipolar Disorder involves a combination of psychotherapy and medication. Psychotherapy, often referred to as talk therapy, includes Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT). These methods of care are beneficial for managing symptoms of BPD and Bipolar Disorder. Medication, such as mood stabilizers, antipsychotics, or antidepressants, may be prescribed based on individual symptoms. Treatment plans should be personalized under the guidance of a mental health professional, and may require adjustments over time.
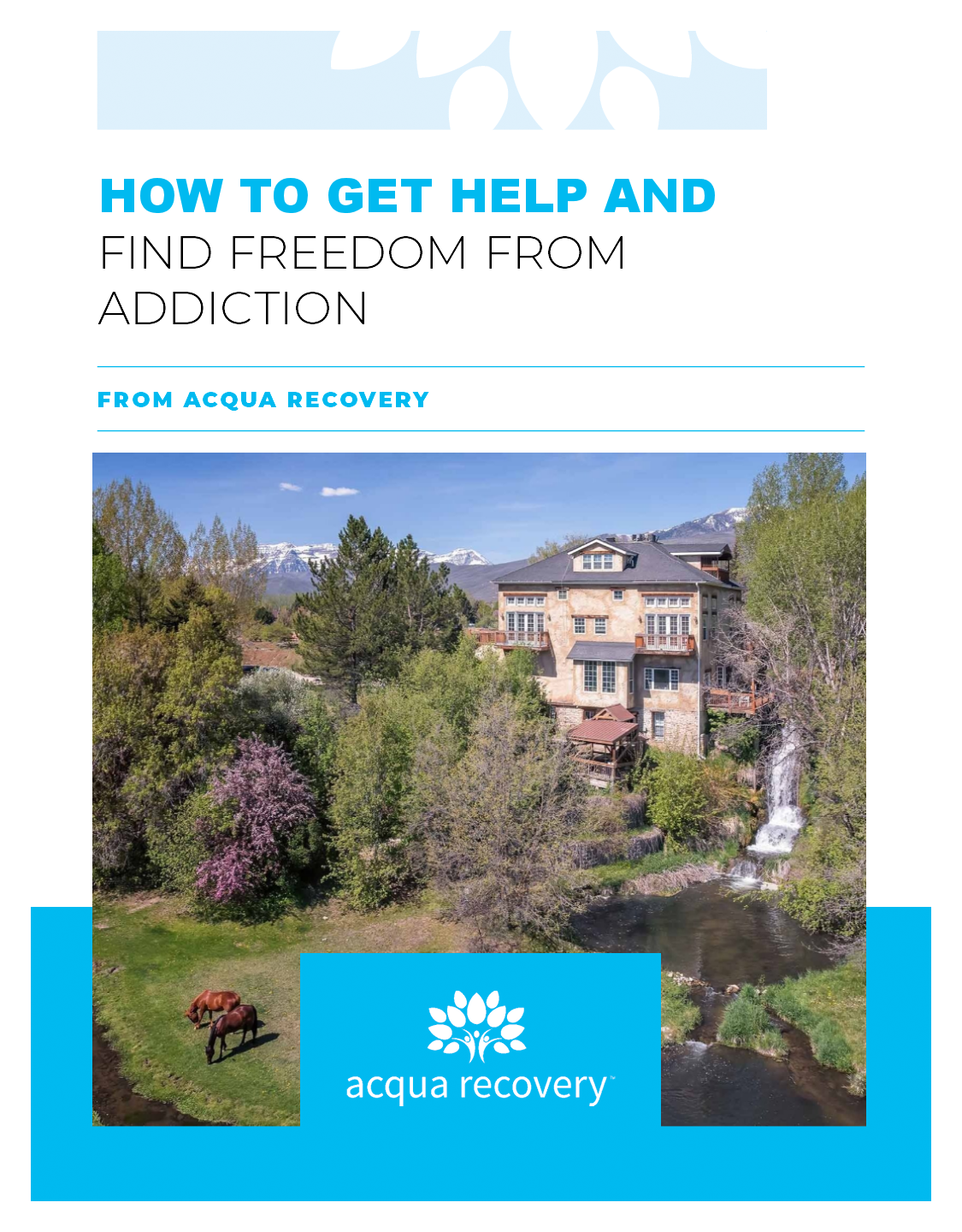
Call Acqua Recovery for Mental Health Treatment in Utah
While both BPD and Bipolar Disorder present with intense emotional shifts and impulsive behaviors, the two are fundamentally distinct conditions. The key differences lie in the nature, duration, and triggers of mood swings, with BPD primarily characterized by variations in mood, self-image, and behavior, and bipolar disorder characterized by periods of depression and mania. Understanding these differences is crucial for accurate diagnosis and effective management.
If you’d like to learn more about how Acqua Recovery can help you overcome your mental health disorder, you can contact us here.