How to Use Your First Health Insurance for Addiction Treatment at Acqua Recovery
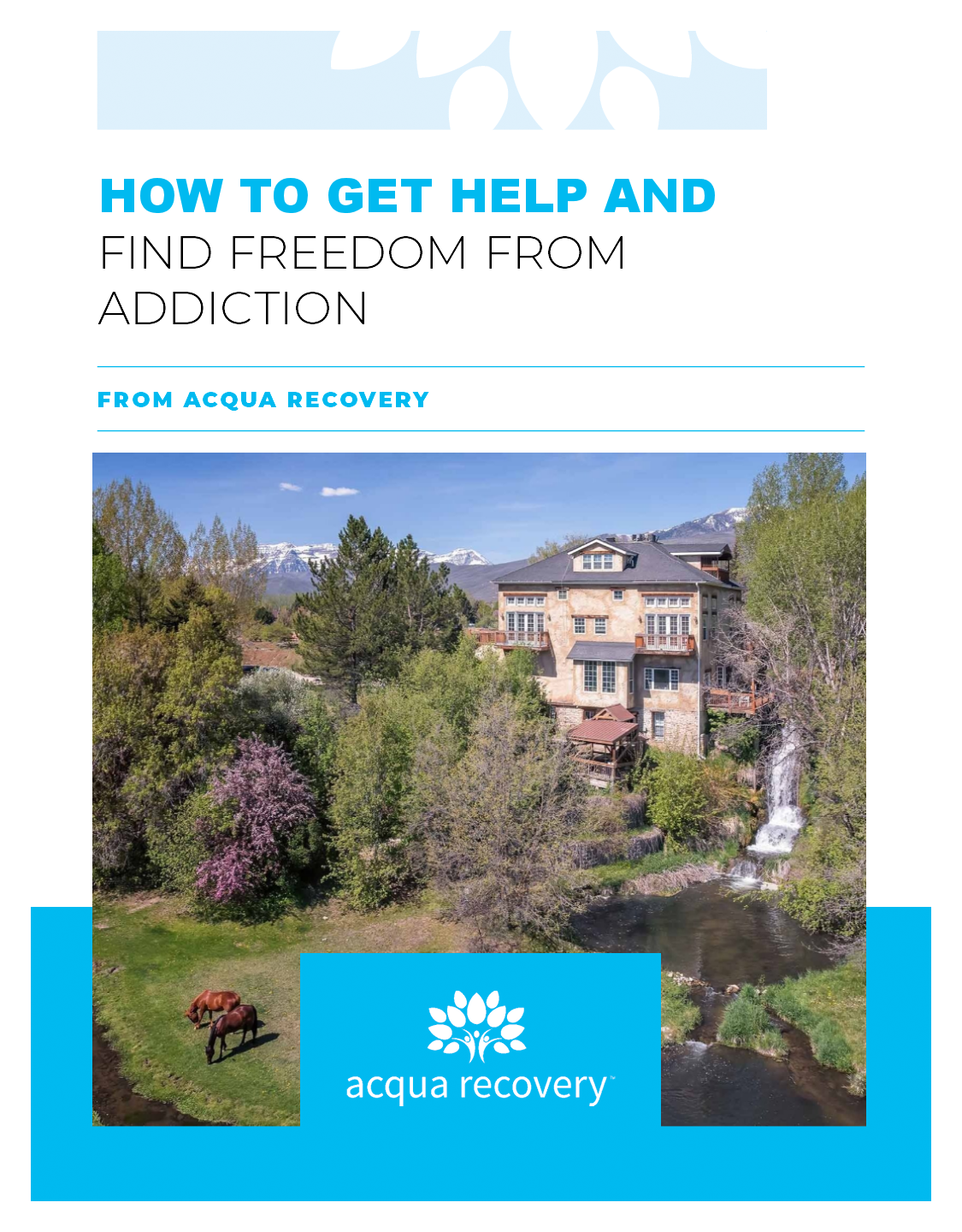
Addiction treatment is an essential part of recovery for individuals struggling with substance abuse. At Acqua Recovery, we understand how difficult it can be to navigate the insurance landscape and find the right provider that meets your needs. We are proud to accept First Health Insurance, a subsidiary of Aetna Inc., as one of our accepted insurance providers.

About First Health Insurance
First Health Insurance is one of the largest national PPO networks, offering coverage for individuals and businesses across the United States. As a subsidiary of Aetna Inc., First Health is backed by the resources and expertise of one of the leading healthcare companies in the country.
Using First Health Insurance at Acqua Recovery
If you or a loved one is seeking addiction treatment, Acqua Recovery can help. Our programs are designed to address a range of substance abuse issues, including alcohol, opiates, cocaine, marijuana, prescription medication addiction, fentanyl, heroin, and meth.
To use your First Health Insurance at Acqua Recovery, simply contact your insurance provider to verify your benefits and eligibility. Our team can also assist you with this process to ensure a smooth admission process.
Programs Offered at Acqua Recovery
Acqua Recovery offers a range of addiction treatment programs to meet the unique needs of each individual. Our evidence-based and holistic approach includes:
- Residential treatment
- Intensive outpatient program (IOP)
- Dual diagnosis treatment
- Aftercare support
Each program is tailored to the individual’s specific needs, and our experienced team of addiction specialists is dedicated to providing compassionate and effective care.
Frequently Asked Questions about Addiction Treatment and Insurance
Q: Will my insurance cover addiction treatment?
A: It depends on your insurance plan. Contact your insurance provider to verify your benefits and eligibility.
Q: What types of addiction treatment programs does Acqua Recovery offer?
A: Acqua Recovery offers medical detoxification, residential treatment, intensive outpatient program (IOP), dual diagnosis treatment, and aftercare support.
Q: Can I use my First Health Insurance at Acqua Recovery?
A: Yes, Acqua Recovery accepts First Health Insurance, a subsidiary of Aetna Inc.
Q: How long does addiction treatment typically last?
A: The length of treatment varies depending on the individual’s needs and progress. Our team works closely with each patient to create a personalized treatment plan that meets their unique needs.
If you or a loved one is struggling with addiction, Acqua Recovery is here to help. Contact us today to learn more about our programs and how we can assist you in your journey towards recovery.
Call or chat with an insurance specialist today.

Dr. Pickrell is a board-certified psychiatrist with interests in addiction and psychiatry. He strives to identify the underlying cause of substance use. His understanding of addiction as the overlapping symptoms of biopsychosocial development is the foundation to his care model. He is committed to helping both patients and families understand that addiction is a treatable medical illness. He has been involved in the treatment of addiction for the last 17 years and completed his residency training at the University of Utah.