Acqua Recovery's Addiction Treatment Programs Covered by MHNet Insurance
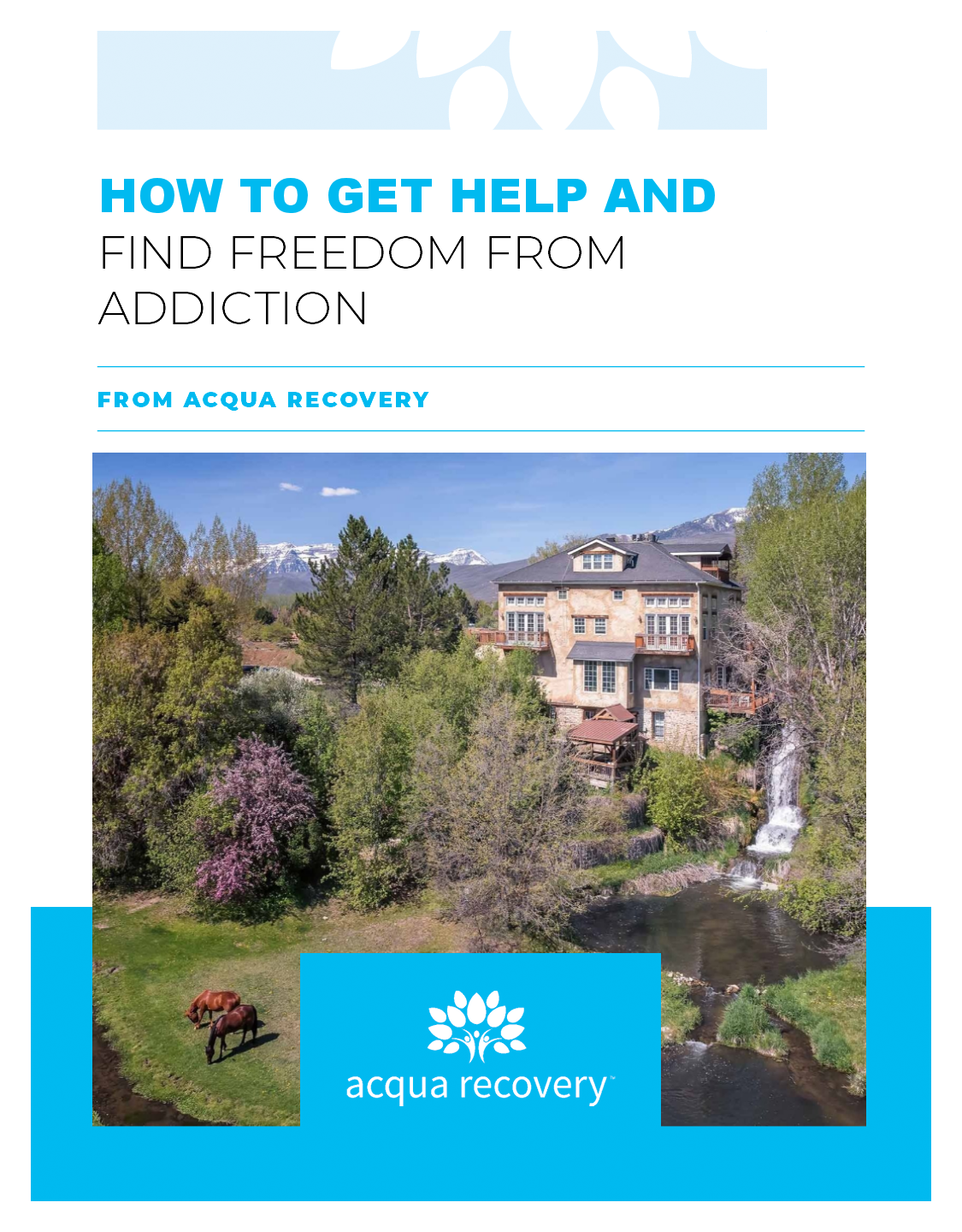
If you or someone you know is struggling with addiction, it can be difficult to know where to turn for help. That’s why Acqua Recovery is here to provide a safe and supportive environment for individuals seeking addiction treatment. At Acqua Recovery, we believe in treating the whole person – mind, body, and spirit – to help our clients achieve lasting recovery.

We are proud to announce that Acqua Recovery’s addiction treatment programs are covered by MHNet Insurance. MHNet, which stands for Managed Health Network LLC, is a behavioral health plan that covers medically necessary mental health services and substance use disorder treatment. This means that if you have MHNet Insurance, you can use it to cover the cost of our programs.
Our Treatment Programs
At Acqua Recovery, we offer a range of evidence-based treatment programs to meet the unique needs of each individual who comes to us for help. Our programs include:
Residential Treatment: Our residential treatment program is designed for individuals who need intensive, round-the-clock care to overcome addiction. During residential treatment, clients live on-site at Acqua Recovery and participate in a variety of therapies and activities.
Intensive Outpatient Treatment: Our intensive outpatient program is ideal for individuals who have completed residential treatment or who do not require 24-hour care. Clients attend therapy and activities at Acqua Recovery during the day and return home in the evenings.
Outpatient Treatment: Our outpatient program is designed for individuals who require less intensive treatment or who have completed a higher level of care. Clients attend therapy and activities at Acqua Recovery on a part-time basis.
Therapies and Activities
In addition to our treatment programs, we offer a variety of therapies and activities to help our clients achieve lasting recovery. Some of these include:
Individual Therapy: One-on-one therapy with a licensed therapist to address underlying issues and develop coping skills.
Group Therapy: Small group sessions to build a sense of community and learn from others.
Family Therapy: Sessions with family members to address issues and rebuild relationships.
Outdoor Therapy: Activities such as hiking, fishing, and kayaking to promote physical and emotional well-being.
Mindfulness and Meditation: Techniques to help clients manage stress and develop a sense of inner peace.
Using MHNet Insurance at Acqua Recovery
If you have MHNet Insurance and are interested in using it to cover the cost of addiction treatment at Acqua Recovery, the first step is to contact us. We will work with you to verify your insurance coverage and determine what treatment programs and services are available to you.
Frequently Asked Questions
Q: What types of addiction does Acqua Recovery treat?
A: Acqua Recovery offers treatment for alcohol, opiates, cocaine, marijuana, prescription medication addiction, fentanyl, heroin, and meth.
Q: How long does treatment at Acqua Recovery last?
A: The length of treatment varies depending on the individual’s needs and progress. Our residential program typically lasts 30-90 days, while our outpatient programs can last up to a year or more.
Q: Will my MHNet Insurance cover the cost of treatment at Acqua Recovery?
A: If you have MHNet Insurance, it may cover some or all of the cost of addiction treatment at Acqua Recovery. We will work with you to verify your insurance coverage and determine what treatment programs and services are available to you.
Don’t let addiction control your life any longer. Contact Acqua Recovery today to learn more about our addiction treatment programs and how we can help you achieve lasting recovery.
Call or chat with an insurance specialist today.

Dr. Pickrell is a board-certified psychiatrist with interests in addiction and psychiatry. He strives to identify the underlying cause of substance use. His understanding of addiction as the overlapping symptoms of biopsychosocial development is the foundation to his care model. He is committed to helping both patients and families understand that addiction is a treatable medical illness. He has been involved in the treatment of addiction for the last 17 years and completed his residency training at the University of Utah.