When exploring treatment options for addiction and co-occurring mental health conditions, you’ll likely encounter two evidence-based therapies that have transformed countless lives: Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT). While both approaches share common roots in cognitive-behavioral principles, they offer distinct pathways to recovery. Understanding the differences between CBT vs DBT can help you or your loved one make informed decisions about which therapy—or combination of therapies—might work best for your unique situation.
What Is Cognitive Behavioral Therapy (CBT)?
Cognitive Behavioral Therapy is a structured, goal-oriented form of psychotherapy that focuses on identifying and changing negative thought patterns and behaviors that contribute to substance use and mental health challenges. Developed by Dr. Aaron Beck in the 1960s, CBT operates on the principle that our thoughts, feelings, and behaviors are interconnected, and by changing our thinking patterns, we can ultimately change our actions and emotional responses.
In addiction treatment, CBT helps individuals recognize the triggers and thought patterns that lead to substance use. Through functional analysis, clients learn to identify high-risk situations and develop healthier coping mechanisms. The therapy emphasizes skill-building techniques such as stress management, problem-solving, and relapse prevention strategies that clients can apply long after treatment ends.
The widespread adoption of CBT speaks to its effectiveness. According to data from the 2020 National Survey of Substance Abuse Treatment Services, 94% of treatment facilities in the United States report using CBT in their substance use disorder programs, making it one of the most commonly utilized evidence-based approaches in the field. This extensive implementation reflects both the therapy’s proven track record and its adaptability to various treatment settings
The Effectiveness of CBT in Addiction Treatment
Research consistently demonstrates CBT’s efficacy in treating substance use disorders. Meta-analyses examining CBT for adult substance use disorders show small but statistically significant effects compared to other treatment conditions, with outcomes comparable to other evidence-based modalities like motivational interviewing and contingency management.
Studies indicate that CBT alone is 50-75% effective in helping individuals overcome depression and anxiety within 5 to 15 sessions—conditions that frequently co-occur with addiction. This dual benefit makes CBT particularly valuable for individuals facing multiple challenges in recovery. Furthermore, approximately 60% of people treated with cognitive behavioral therapy for addiction can maintain their recovery for a year, demonstrating the therapy’s lasting impact beyond the immediate treatment period.
The strength of CBT lies in its emphasis on developing practical coping skills that extend far beyond the therapy session. Clients learn to identify their personal triggers, challenge distorted thinking patterns, and implement healthier behavioral responses when faced with stressful situations or cravings.
What Is Dialectical Behavior Therapy (DBT)?

Dialectical Behavior Therapy, developed by Dr. Marsha Linehan in the late 1980s, was originally designed to treat individuals with Borderline Personality Disorder who struggled with chronic suicidal ideation. DBT has since expanded to treat a range of conditions, including substance use disorders, eating disorders, and other conditions characterized by emotional dysregulation.
DBT combines cognitive-behavioral techniques with mindfulness practices and acceptance strategies. The term “dialectical” refers to the therapy’s focus on balancing acceptance (accepting yourself as you are) with change (working to modify problematic behaviors). This balanced approach makes DBT particularly effective for individuals who experience intense emotional responses and have difficulty managing their emotions without turning to substances.
The therapy is structured around four core skill modules: mindfulness (staying present and aware), emotion regulation (managing intense feelings), distress tolerance (surviving crises without making things worse), and interpersonal effectiveness (maintaining healthy relationships and boundaries). These skills provide a comprehensive toolkit for navigating the complex emotional landscape of recovery.
The Effectiveness of DBT in Addiction Treatment

DBT has demonstrated significant effectiveness in treating substance use disorders, particularly when combined with other treatment modalities. Research shows that DBT groups achieve statistically significantly better outcomes than comparison groups in increasing substance abstinence, with effect sizes considered medium to large.
After 6 months of DBT treatment, 46% of people showed healthier behavior patterns, and after a year, 51% of individuals showed improved behavior patterns and lifestyles. These improvements extend beyond just substance use, encompassing overall emotional regulation and quality of life.
One of DBT’s unique strengths is its effectiveness with individuals who have co-occurring mental health conditions. The therapy was specifically designed to address emotional dysregulation—a core issue underlying many substance use disorders. This makes DBT particularly valuable for clients who use substances as a way to cope with overwhelming emotions or who have struggled to engage successfully with other treatment approaches.
Key Differences: CBT vs DBT

While both therapies share cognitive-behavioral foundations, several important distinctions set them apart:
- Focus and Approach: CBT primarily targets changing negative thought patterns and behaviors through structured cognitive techniques and behavioral interventions. DBT, while incorporating these elements, places greater emphasis on acceptance, validation, and managing intense emotions through mindfulness and distress tolerance skills.
- Structure and Duration: CBT tends to be more time-limited and problem-focused, often conducted over 12-16 weeks of individual therapy sessions. DBT typically involves a more comprehensive structure that includes individual therapy, group skills training, phone coaching for crisis situations, and consultation teams for therapists—often lasting six months to a year or longer.
- Emotional Regulation: While CBT addresses emotional responses, DBT places particular emphasis on teaching specific skills for managing extreme emotional states. The distress tolerance module in DBT specifically prepares clients to survive crisis situations without engaging in destructive behaviors like substance use.
- Target Population: CBT is broadly effective for various mental health conditions and substance use disorders. DBT was specifically developed for individuals with severe emotional dysregulation, chronic suicidal ideation, self-harm behaviors, and those with Borderline Personality Disorder, though its applications have expanded significantly.
- Therapeutic Relationship: Both therapies value the therapeutic relationship, but DBT explicitly emphasizes validation and the dialectical balance between acceptance and change. Therapists work to validate clients’ experiences while simultaneously helping them change problematic behaviors.
Which Therapy Is Right for You?

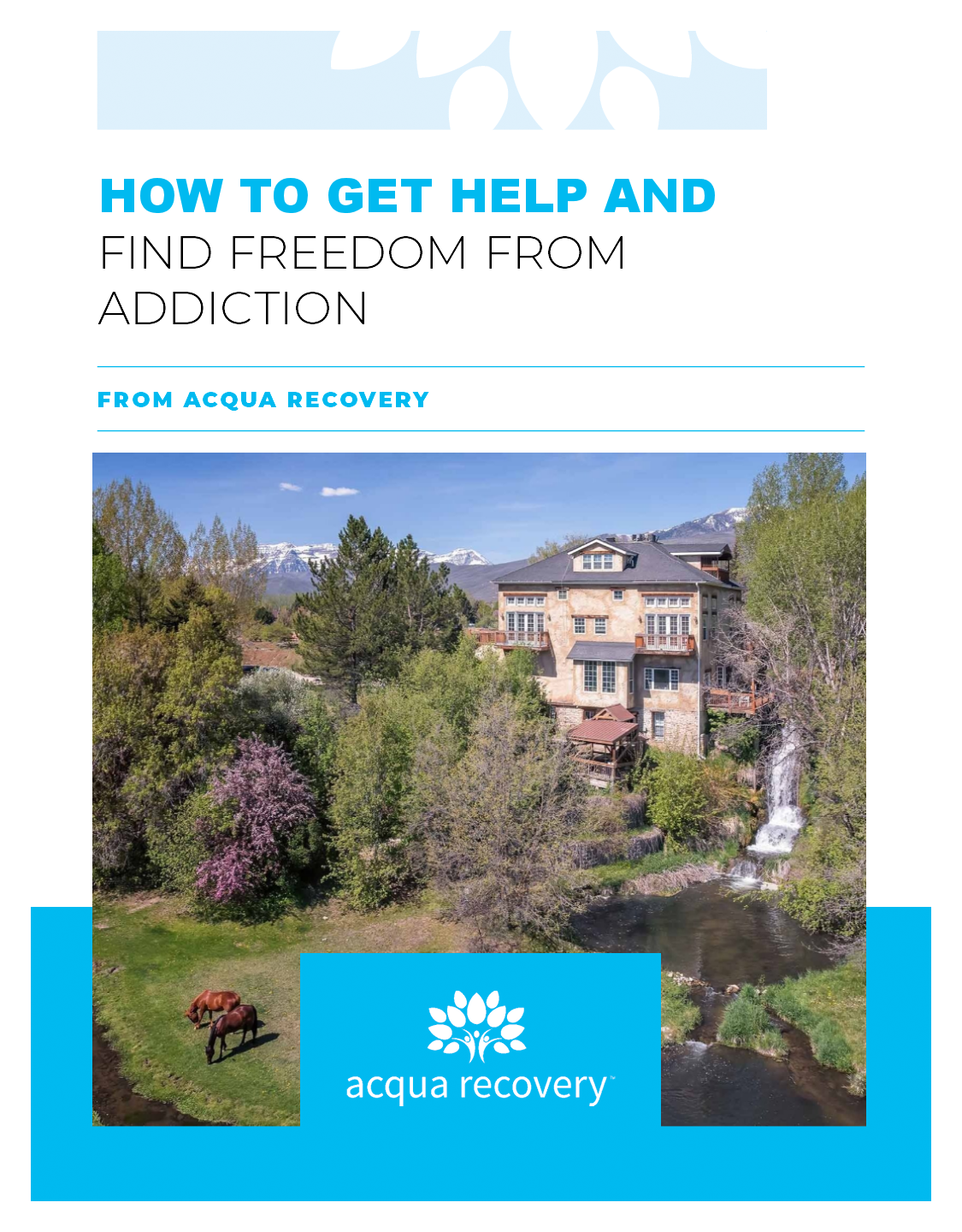
The question of CBT vs DBT isn’t always about choosing one over the other. Many comprehensive treatment programs, including those at Acqua Recovery, integrate both approaches to provide the most effective care possible.
CBT may be particularly beneficial if you’re looking for structured, problem-focused therapy that helps you identify and change specific thought patterns and behaviors contributing to substance use. It’s excellent for individuals who respond well to cognitive techniques and are working to develop practical coping skills for relapse prevention.
DBT might be more appropriate if you experience intense emotional responses, struggle with emotion regulation, have a history of self-harm or suicidal thoughts, or have found it difficult to engage successfully with other treatment approaches. The comprehensive skill-building approach of DBT can be especially helpful for individuals who need support managing crisis situations and interpersonal challenges.
However, many individuals benefit from elements of both therapies. At Acqua Recovery, our integrated approach to addiction treatment combines evidence-based therapies like CBT and DBT with other modalities such as EMDR, Internal Family Systems (IFS), and trauma-informed care to create personalized treatment plans that address each client’s unique needs.
Moving Forward in Your Recovery Journey
Understanding the differences between CBT vs DBT is an important step in making informed decisions about your treatment. Both therapies offer powerful tools for overcoming addiction and building a healthier, more balanced life. The most effective approach often involves combining elements of both therapies, along with other evidence-based treatments, to address the full complexity of addiction and mental health challenges.
Recovery is a deeply personal journey, and the right therapeutic approach will depend on your individual circumstances, mental health history, and treatment goals. By working with experienced clinicians who can assess your needs and design a personalized treatment plan, you can access the specific therapies and support services that will give you the best chance for long-term success.
If you’re ready to explore how CBT, DBT, or a combination of evidence-based therapies can support your recovery journey, contact Acqua Recovery today. Our compassionate admissions team can answer your questions, verify your insurance, and help you take the first step toward lasting healing and transformation. Whether you’re seeking treatment for yourself or a loved one, we’re here to guide you toward the evidence-based care that can make all the difference in your recovery.
FAQS
Yes, many comprehensive addiction treatment programs, including Acqua Recovery, integrate both CBT and DBT approaches. Rather than choosing one over the other, treatment teams often combine elements of both therapies to create a personalized treatment plan that addresses your unique needs. This integrated approach allows you to benefit from CBT’s structured problem-solving techniques while also developing DBT’s emotion regulation and distress tolerance skills.
The timeline for seeing results varies by individual and the complexity of your situation. CBT is typically more time-limited, with many people experiencing improvements within 5 to 15 sessions. DBT programs generally run longer, from six months to a year or more, as they involve comprehensive skills training across four core modules. However, many clients report feeling better equipped to manage cravings and emotions within the first few weeks of either therapy.
No, while DBT was originally developed to treat Borderline Personality Disorder, it has proven effective for a wide range of conditions including substance use disorders, eating disorders, depression, anxiety, PTSD, and other conditions involving emotional dysregulation. DBT’s skills-based approach benefits anyone who struggles with intense emotions, impulse control, or managing relationships during recovery.
Both CBT and DBT have strong evidence supporting their effectiveness in treating addiction. CBT demonstrates small to statistically significant effects and is used in 94% of U.S. treatment facilities. DBT shows medium to large effect sizes for substance abstinence, particularly for individuals with co-occurring emotional regulation challenges. The “better” choice depends on your individual circumstances, mental health history, and whether you struggle more with thought patterns (CBT’s strength) or intense emotions (DBT’s strength).